By Stacey Spencer, Senior Product Marketing Manager, Endosurgical, FUJIFILM Healthcare Americas Corporation
Fujifilm’s ELUXEO® Vision innovative technology was recently highlighted at the American Society of Colon and Rectal Surgeons (ACSRS) annual meeting, the leading educational event in the field of colon and rectal surgery. The symposium presented by key opinion leader Dr. Sang Lee, Charles and Carolyn Costello Chair in Colorectal Diseases, Professor and Chief of Colorectal Surgery – University of Southern California, described how this unique technology can alter the surgical plan, leading to tangible improvements in patient care.
Anastomotic leaks, a well-known — and the most devastating— complication of colorectal surgery,[i] are linked to several negative outcomes and risk factors, including increased morbidity, mortality, extended hospitalizations, and increased economic burden.[ii] The occurrence of anastomotic leaks can also increase the rate of local recurrence and reduces short and long-term patient survival.[iii],[iv] Tissue perfusion at the surgical site is a key surgery-related factor that can affect anastomotic outcomes.[ii] ,[v] The ability to detect ischemic anastomotic tissue during surgery is therefore key in assessing tissue viability in real-time, reducing complications, patient burden, and cost.

Tissue blood perfusion in endoscopic interventions is typically evaluated using indocyanine green (ICG) fluorescence to aid in visualization of blood vessels and other anatomical structures. Although widely used, both the technique’s inherent limitations as well as those introduced by inter-user variability — such as differences in bioavailability due to patient weight and other factors, dye contraindications (allergy, pregnancy), inconsistent dye administration, bias caused by ICG injection/read timing, and camera distance/placement discrepancies — can lead to highly subjective results. Studies on the utility of ICG in intraoperative decision-making have shown varying results: although some report that ICG use is associated with lower odds of anastomotic leaks, experts urge that optimal use requires careful dosage and timing considerations, appropriate training, and careful patient selection,[vi],[vii],[viii],[ix],[x],[xi] and call for technological improvements that provide real-time visualization with standardized, quantitative parameters.[xii],[xiii],[xiv]
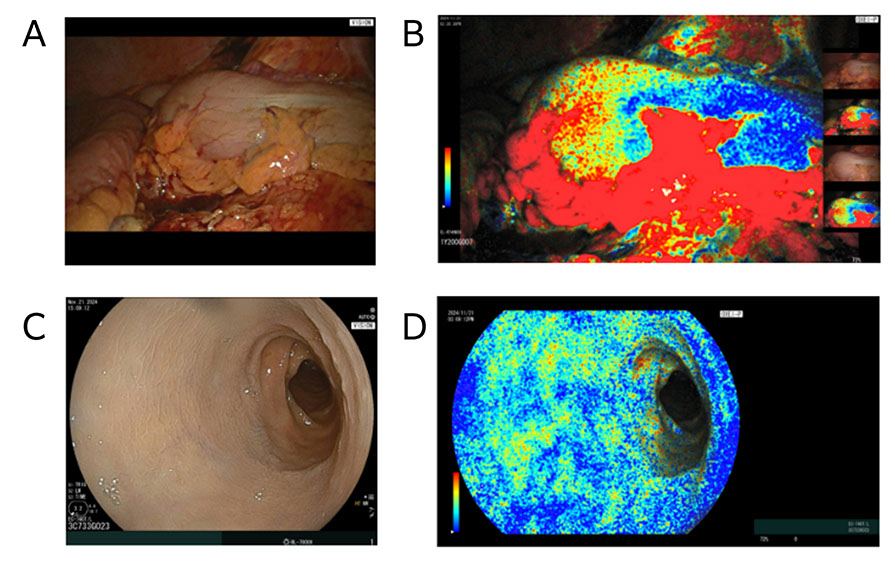
ELUXEO Vision harnesses novel light and image processing technology to measure tissue oxygen saturation (StO2) levels in numerical data points, helping surgeons with real-time, quantitative tissue viability evaluation. Multiple imaging modes provide additional information that can aid in clear identification of demarcation lines while monitoring the change of tissue oxygenation levels over time. The ELUXEO Vision can be used in both endoscopic and laparoscopic procedures, expanding the range of applications and optimizing space in the operating room.
“The ELUXEO Vision system provides valuable, quantitative data on tissue oxygenation at and near anastomotic sites, complementing traditional white light endoscopy and leak tests”
Dr. Lee’s study used ELUXEO Vision both endoscopically and laparoscopically to evaluate StO2 in 24 patients undergoing left-sided colectomy and anastomosis. The ELUXEO Vision was a viable and objective method for intraoperative assessment of tissue oxygen saturation in both serosal and mucosal sides in real time and without the use of dyes. In particular, the ELUXEO Vision had a significant impact on operative plans in one patient, where a modification of the planned anastomosis site based on tissue oxygen findings helped mitigate potential anastomotic leak complications (see figure). “The ELUXEO Vision system provides valuable, quantitative data on tissue oxygenation at and near anastomotic sites, complementing traditional white light endoscopy and leak tests,” Dr. Lee concluded.
ELUXEO Vision was granted FDA Breakthrough Device Designation in September 2020 and received FDA 510(k) clearance in June 2021. Early trials showing the technology’s potential to transform the field of surgical endoscopy were first highlighted in a talk at the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) 2023 annual meeting. Dr. Lee’s study is the first to show supporting clinical data highlighting how use of ELUXEO Vision can alter the surgical plan and may result in more favorable long-term outcomes.
 Stacey Spencer, Senior Product Marketing Manager, Endosurgical, FUJIFILM Healthcare Americas Corporation
Stacey Spencer, Senior Product Marketing Manager, Endosurgical, FUJIFILM Healthcare Americas Corporation
[i] Chiarello MM, Fransvea P, Cariati M, Adams NJ, Bianchi V, Brisinda G. 2022. Anastomotic leakage in colorectal cancer surgery. Surg Oncol 40:101708, PMID: 35092916.
[ii] Zhao Y, Li B, Sun Y, Liu Q, Cao Q, et al. 2022. Risk factors and preventive measures for anastomotic leak in colorectal cancer. Technol Cancer Res Treat 21:15330338221118983, PMID: 36172641.
[iii] Turrentine FE, Denlinger CE, Simpson VB, Garwood RA, Guerlain S, et al. 2015. Morbidity, mortality, cost, and survival estimates of gastrointestinal anastomotic leaks. J Am Coll Surg 220(2):195-206, PMID: 25592468.
[iv] Ha GW, Kim JH, Lee MR. 2017. Oncologic impact of anastomotic leakage following colorectal cancer surgery: A systematic review and meta-analysis. Ann Surg Oncol 24(11):3289-3299, PMID: 28608118.
[v] Renna MS, Grzeda MT, Bailey J, Hainsworth A, Ourselin S, et al. 2023. Intraoperative bowel perfusion assessment methods and their effects on anastomotic leak rates: Meta-analysis. Br J Surg 110(9):1131-1142, PMID: 37253021.
[vi] Son GM, Kwon MS, Kim Y, Kim J, Kim SH, Lee JW. 2019. Quantitative analysis of colon perfusion pattern using indocyanine green (ICG) angiography in laparoscopic colorectal surgery. Surg Endosc 33(5):1640-1649, PMID: 30203201.
[vii] Emile SH, Khan SM, Wexner SD. 2022. Impact of change in the surgical plan based on indocyanine green fluorescence angiography on the rates of colorectal anastomotic leak: A systematic review and meta-analysis. Surg Endosc 36(4):2245-2257, PMID: 35024926.
[viii] Liu RQ, Elnahas A, Tang E, Alkhamesi NA, Hawel J, et al. 2022. Cost analysis of indocyanine green fluorescence angiography for prevention of anastomotic leakage in colorectal surgery. Surg Endosc 36(12):9281-9287, PMID: 35290507.
[ix] Khalafi S, Botero Fonnegra C, Reyes A, Hui VW. 2024. Developments in the use of indocyanine green (ICG) fluorescence in colorectal surgery. J Clin Med 13(14):4003, PMID: 39064041.
[x] De Simone B, Abu-Zidan FM, Boni L, Castillo AMG, Cassinotti E, et al; ICG-Fluorescence guided emergency surgery consensus participants; Catena F. 2025. Indocyanine green fluorescence-guided surgery in the emergency setting: the WSES international consensus position paper. World J Emerg Surg 20(1):13, PMID: 39948641.
[xi] Rinne JKA, Huhta H, Pinta T, Turunen A, Mattila A, et al. 2025. Indocyanine green fluorescence imaging in prevention of colorectal anastomotic leakage: A randomized clinical trial. JAMA Surg 160(5):486-493, PMID: 40042831.
[xii] Larsen PO, Nerup N, Andersen J, Dohrn N, Klein MF, et al. 2023. Anastomotic perfusion assessment with indocyanine green in robot-assisted low-anterior resection, a multicenter study of interobserver variation. Surg Endosc 37(5):3602-3609, PMID: 36624218.
[xiii] Pollmann L, Juratli M, Roushansarai N, Pascher A, Hölzen JP. 2023. Quantification of indocyanine green fluorescence imaging in general, visceral and transplant surgery. J Clin Med 12(10):3550, PMID: 37240657.
[xiv] Preziosi A, Cirelli C, Waterhouse D, Privitera L, De Coppi P, Giuliani S. 2024. State of the art medical devices for fluorescence-guided surgery (FGS): technical review and future developments. Surg Endosc 38(11):6227-6236, PMID: 39294317.